Understanding the Causes of Horner Syndrome: A Comprehensive Guide
Horner syndrome is an uncommon disorder that damages the nerves regulating face and ocular movements. Among the several symptoms it can bring about are ptosis (drooping eyelid), miosis (constricted pupil), anhidrosis (lack of sweating), and enophthalmosis (sunken eye). Correct diagnosis and treatment depend on an awareness of the underlying reasons for Horner Syndrome.
The disorder results from a disturbance of the sympathetic nerve pathway in charge of these processes. It can cause obvious changes in appearance and impact one side of the face. Several elements, from damage to underlying medical disorders, can help produce Horner Syndrome. This article will discuss the several causes and risk factors of Horner Syndrome to help you better grasp this complicated neurological condition.
Common Causes Of Horner Syndrome
Below are the common causes of Horner Syndrome, which can result from various conditions affecting the sympathetic nerve pathway.
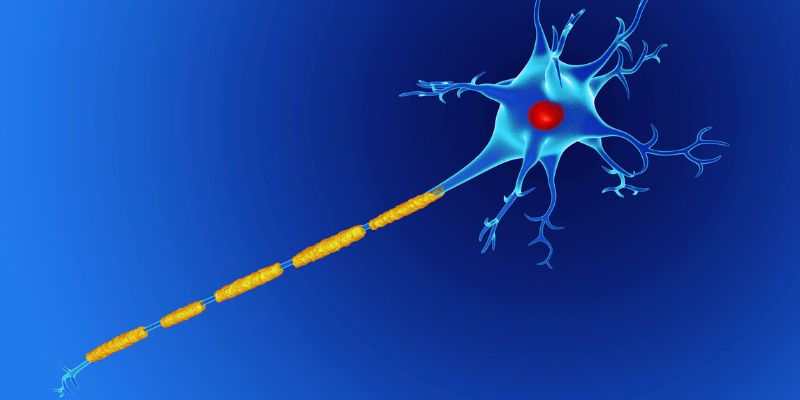
Nerve Pathway Disruption:
A disturbance in the sympathetic nerve system, which passes into the neck and the eye from the brain via the spinal cord, usually causes Horner Syndrome. However, Horner Syndrome can arise from any injury or disturbance of this neural system. The sympathetic nerves regulate the muscles surrounding the eye, preserving the normal pupil and eyelid position. Affected nerves can produce symptoms, including a drooping eyelid, tiny pupil, and decreased perspiration on one side of the face.
Brainstem Lesions
Additionally, Horner syndrome is caused by a brainstem lesion. The brainstem regulates the signals following the sympathetic route. Any injury to the brainstem resulting from a stroke, tumor, or other disorder can interfere with the brain's transmission to the eye muscles. It can bring forth the usual Horner Syndrome symptoms. Though less common, brainstem lesions can be rather severe and should be seen immediately by a doctor.
Neck Injuries or Tumors
Horner Syndrome can also result from neck area injuries or malignancies. Before ever reaching the eyes, the sympathetic nerves pass via the neck. Trauma like a medical operation or vehicle accident can compromise these nerves. Furthermore, compressing or invading the nerve pathway are cancers in the neck, particularly those close to the sympathetic nerves. Horner syndrome results from this compression, which interferes with normal nerve transmission.
Carotid Artery Disease
The carotid artery runs across the neck and feeds the brain. If it becomes blocked or narrowed, blood flow to the nerves in charge of the eye may change. Horner Syndrome, sometimes known as carotid artery disease, can result from this disorder. Ischemia—a lack of oxygen—caused by the disturbance in blood flow might harm the neurons. Older persons or those with diabetes and other cardiovascular risk factors typically exhibit this.
Congenital Horner Syndrome
Certain people have congenital causes for their Horner Syndrome. In certain situations, the problem could result from improper development of the neural route during childbirth. Usually found in infancy or early childhood, congenital Horner syndrome. Though the symptoms could be less severe in certain situations, ptosis, miosis, and anhidrosis abound. Sometimes, congenital Horner syndrome is linked to other developmental disorders. Hence, doctors should constantly observe these patients.
Multiple Sclerosis (MS)
Multiple sclerosis, a chronic illness, compromises the central nervous system. It happens as the immune system targets the protective layer surrounding nerve fibers. Lesions in several brain and spinal cord areas may follow. Horner syndrome can result from MS compromising the part of the brain that regulates the sympathetic nerve route. In those who already have other neurological symptoms, such as weakness or trouble walking, MS is more likely to produce Horner Syndrome.
Tumors in the Chest or Upper Body
Horner Syndrome can also be brought on by some upper body or chest malignancies. As they develop, these tumors could either penetrate or compress the sympathetic nerve route. Lung cancer, particularly a Pancoast tumor, can, for instance, compromise the sympathetic nerves. Another kind of tumor that can produce Horner Syndrome is lymphoma, a lymphatic system cancer. Sometimes tumors that metastasize—spread—from other body parts can also produce Horner Syndrome symptoms by entering the sympathetic nerves.
Migraines and Headaches
In some instances, Horner Syndrome has been linked to migraines and other forms of headache. Although the precise process is unknown, it is thought that some forms of headaches can irritate the sympathetic nerve system, producing symptoms akin to those of Horner Syndrome. These headaches can cause a brief disturbance of nerve activity that would cause the pupil to constrict and the eyelid to drop. Usually, this type of Horner Syndrome is reversible once the headache disappears.
Surgical Complications
If the sympathetic nerves are injured, surgical operations involving the neck or upper chest might cause Horner syndrome. It could happen during procedures for disorders like thyroid problems, lung disease, or vascular concerns. Rare surgical problems can disrupt the nerve route and cause Horner Syndrome to develop. Knowing this risk, surgeons minimize nerve damage during such operations.
Infections
Some infections—especially those affecting the brain or spinal cord—may potentially cause Horner Syndrome. For instance, inflammation in sections of the brainstem regulating the sympathetic nerve route can be brought on by infections such as meningitis or encephalitis. The usual Horner Syndrome symptoms are brought on by this inflammation, upsetting the signals headed to the eyes. Though less often occurring reasons, infections can nonetheless be a contributing component.
Other Rare Causes
Other less common causes of Horner Syndrome are genetic problems, trauma, or vascular abnormalities. These disorders can cause different disturbances in the neural pathways, resulting in symptoms. Some of these reasons might be unclear and would call for further investigation and testing.
Conclusion:
Disorders in the sympathetic nerve circuit regulating eye and face motions produce Horner syndrome. Among the several causes include nerve injury, brainstem lesions, neck injuries, and several disorders like multiple sclerosis. Furthermore, contributing to its growth are tumors, carotid artery disease, and even migraines. Although some cases are hereditary, others result from outside events, including infections or surgical complications. Manage the symptoms and stop more consequences with early diagnosis and treatment. If you show any symptoms of Horner Syndrome, you should see a healthcare provider for appropriate assessment and treatment.











